For anyone involved in primary care, understanding the ins and outs of aortic dissection is crucial. Let’s delve into the recent webinar that took this subject head-on, aiming to enrich the primary care community.
Improving Cardiovascular Care
On 18th July 2023, the South London Cardiovascular Network, in collaboration with the Aortic Dissection Charitable Trust, hosted an hour-long webinar on aortic dissection. Specifically crafted for primary care staff, the event provided crucial knowledge on diagnosis, management, and patient care related to aortic dissection. The event was recorded to ensure accessibility for all.
Deepening Understanding
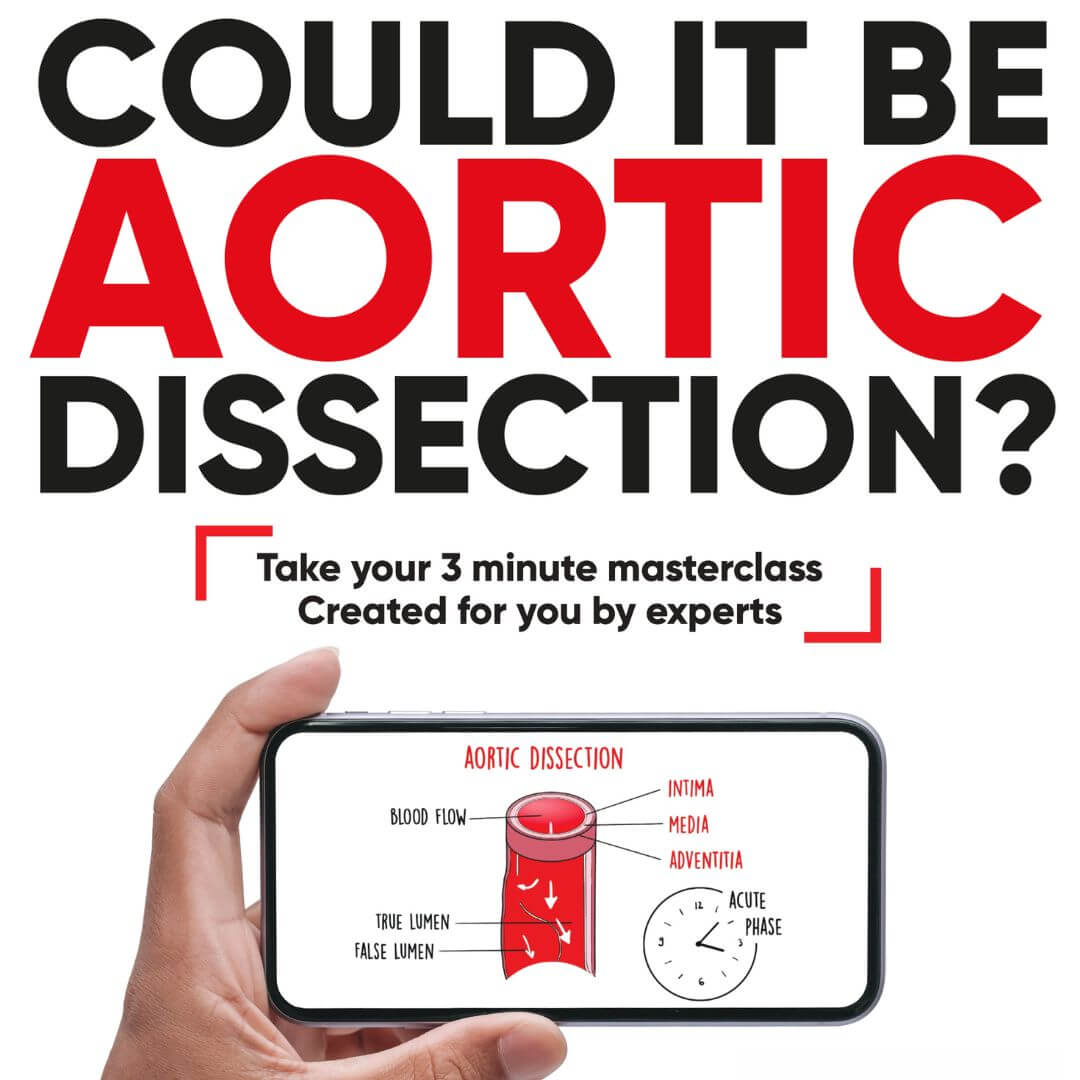
This webinar was more than just a virtual meet-up; it was a deep dive into the crucial tool – the Aortic Dissection Field Guide for Primary Care. This document and its accompanying video guide provide support to achieve treatment consistency across the patient care journey. This collaboration with the PCCS is anchored in GP education, advocacy for policy change, and driving research.
Significant contributions to the guide came from professionals in the field. Dr Victoria McKay, Consultant Clinical Geneticist from Liverpool Heart and Chest Hospital NHS Foundation Trust, and Dr Bejal Pandya, Consultant Cardiologist at Barts Health NHS Foundation Trust, both lent their extensive expertise to the guide.
The Role of the South London Cardiovascular Network
Established in 2018, following an NHS England review, the South London Cardiovascular Network (SLCN) has been active in enhancing cardiac care standards. AortaEd events like these play a pivotal role in equipping primary care staff with the latest best practices and providing access to subject matter experts. Such sessions empower healthcare professionals to provide a higher standard of care for patients and families grappling with aortic dissection.

“At age 13, I was diagnosed with Marfan Syndrome. By 35, I had an aortic root replacement. Then, in 2012, two weeks before my 40th birthday, I felt a ripping sensation in my chest, like a zip being undone from top left down to bottom right, followed by intense pain. Despite initial tests showing no issues, my dad urged me to see my GP. The doctor promptly got me to a different hospital where I was diagnosed with a type B aortic dissection. After years of monitoring and another major surgery in 2020 where my entire aorta was replaced with a Dacron graft, I’m now thankfully fully recovered and living a healthy life again.”

“Joanne’s story highlights the difficulty of diagnosing aortic dissection and the crucial need for long-term follow-up. Patients’ post-dissection need specialised annual MRI scans of the aorta, ensuring blood pressure is controlled and any secondary prevention is in place. If under 55, they may have an inherited risk of aortic dissection which could affect their family, thus requiring genetic screening. Notably, almost half of such patients experience post-traumatic stress disorder, making counselling essential.”
“In my 35 years as a GP, I’ve seen two cases of thoracic dissection. The symptoms include chest and back pain, a ripping or tearing sensation, and vomiting. Pulse deficit and differences in blood pressure between arms are key indicators. Those below 55, with connective tissue disease, or a family history of aortic dissection should undergo genetic assessments and aortic imaging. Primary care follow-up revolves around managing hypertension with a target BP of less than 130/80, although some suggest even lower. Beta-blockers are commonly used for treatment. Notably, 40% of individuals post-dissection experience post-traumatic stress disorder, underscoring the need for mental health support. In fact, a study indicated a significant change in activity post-dissection, with over 75% reporting a negative impact on their lifestyle, and around a third reporting depression.”
Webinar Q&A
-
Could you elaborate on the modern approach to managing hypertension?
There’s a shift towards home blood pressure monitoring, which began notably during the COVID period. This method is found to be more accurate than one-off measurements taken during surgeries. The goal for in-surgery blood pressure is typically 140/90. However, for home monitoring, the aim should be an average of 135/85.
-
If there's a family history of aortic dissection, what do genetic tests screen for?
(Graham) Before testing, patients typically undergo counselling due to the significant implications of identifying an “at-risk” gene. The test itself involves taking a saliva sample and screening for approximately 30 genes associated with aortic dissection. If a concerning gene is detected, especially if there’s a direct family history, we might contemplate prophylactic surgery.
(Jim) To elaborate, primary care has the capacity to refer directly to genetic departments. The patient may then interact with specialist nurses, some of whom are experts in cardiovascular genetics.
-
Are people referred to Cardiac Rehab after an aortic dissection?
(Graham) In my experience, Cardiac Rehab is primarily reserved for patients who’ve undergone coronary artery bypass surgery or have had myocardial infarctions. Aortic dissection patients aren’t typically included.
(Jim) That’s right. Specific groups, like those who’ve had valve surgeries or myocardial infarctions, are often prioritized. We’re also trying to extend this service to heart failure patients due to its proven cost-effectiveness.
-
Regarding post-aortic dissection surgery, what blood pressure should we aim for?
(Graham) Guidelines from Europe and America recommend aiming for 130/80. Research indicates that the risk of aortic dissection directly correlates with blood pressure, meaning higher blood pressure equals a higher risk.
(Jim) Precisely. And while lower blood pressure is ideal, it’s crucial to maintain a balance, especially in older populations, to avoid risks such as postural hypotension.
Join Future Events
This webinar was an illuminating and impactful event that resonated with the primary care community. The collaborative endeavours by the South London Cardiovascular Network and the Trust are a significant step forward in arming healthcare professionals with the vital knowledge and tools needed to tackle this complex condition.
Our commitment to elevating the standard of care for aortic dissection patients remains steadfast, and we have a robust lineup of future AortaEd events in the pipeline. Each planned event aims to continue deepening the understanding, broaden awareness and bring even more expertise to the table. Together, we will continue to empower our primary care community, drive research, and advocate for policy changes that can make a difference in the lives of those affected by aortic dissection. Keep an eye out for upcoming announcements.