Aortic Dissection Explained
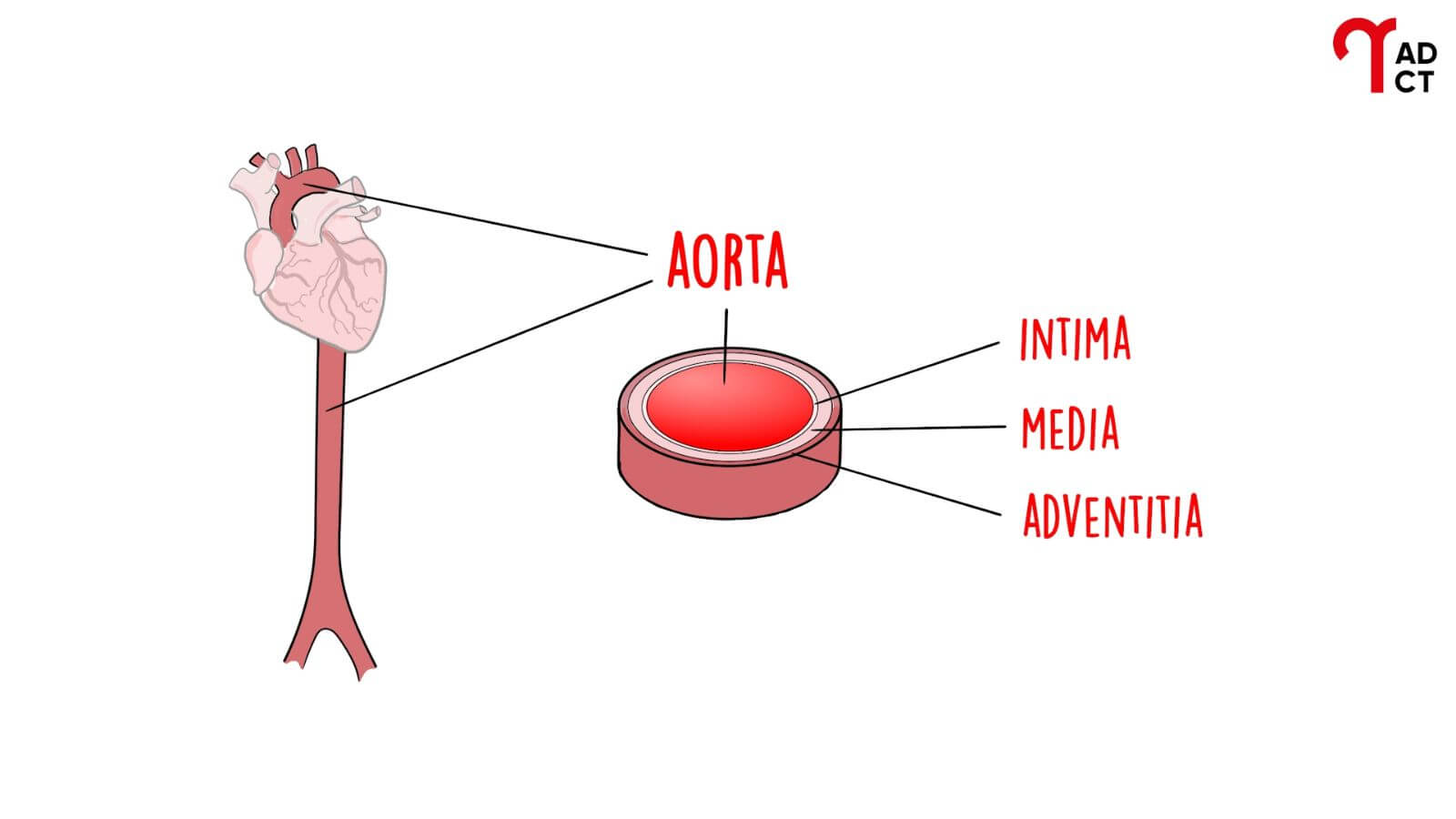
The Aorta
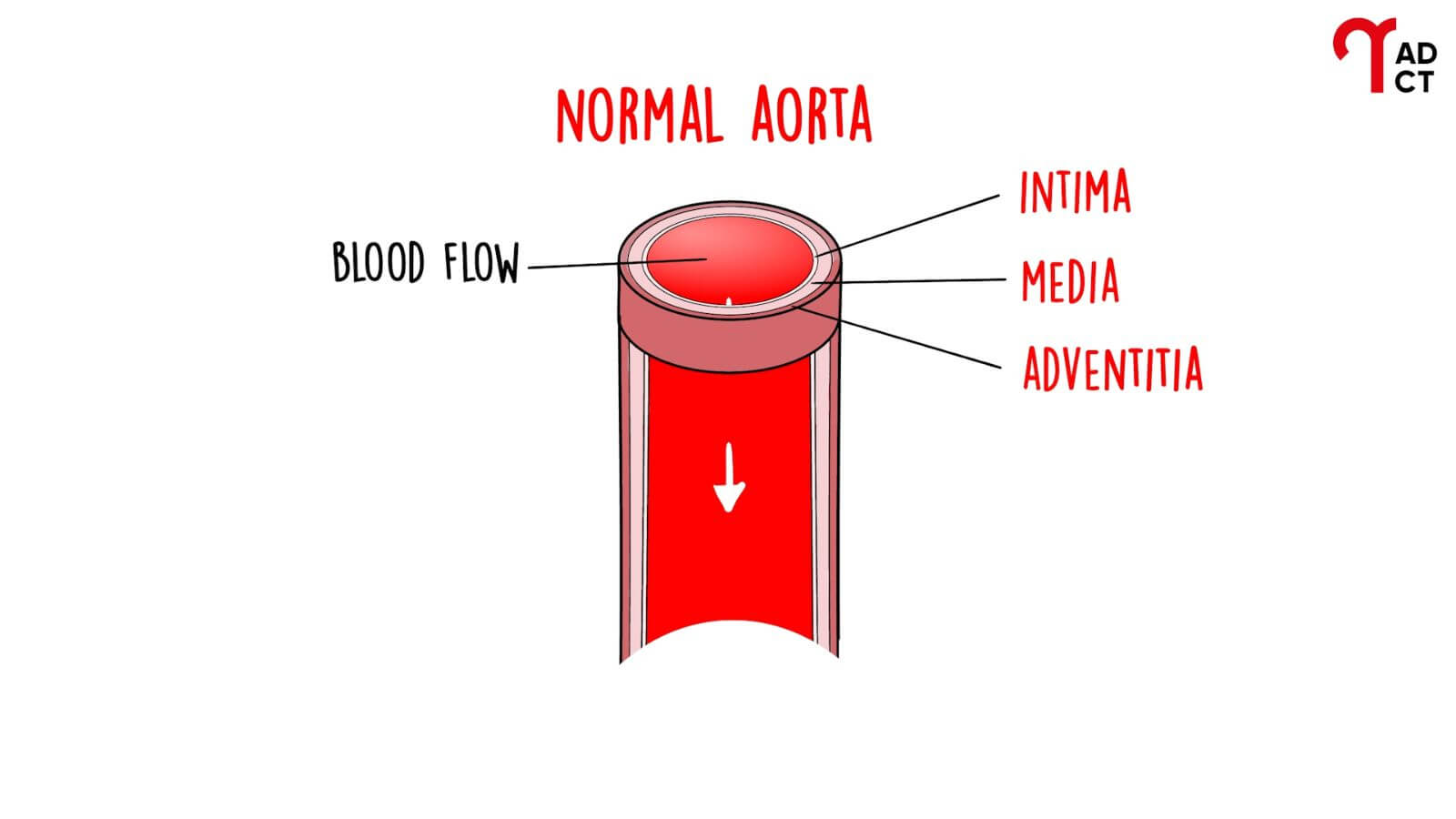
The aorta is the major artery in the body. It carries blood from the heart that goes to all organs. The first part of the aorta leaves the heart and goes up in the front of the chest towards the neck. Here it curves backwards to descend in the back. The aorta then travels down through the chest and abdomen before dividing into the arteries that supply the legs. The aortic wall has three layers: intima, media and adventitia.
Aortic Dissection
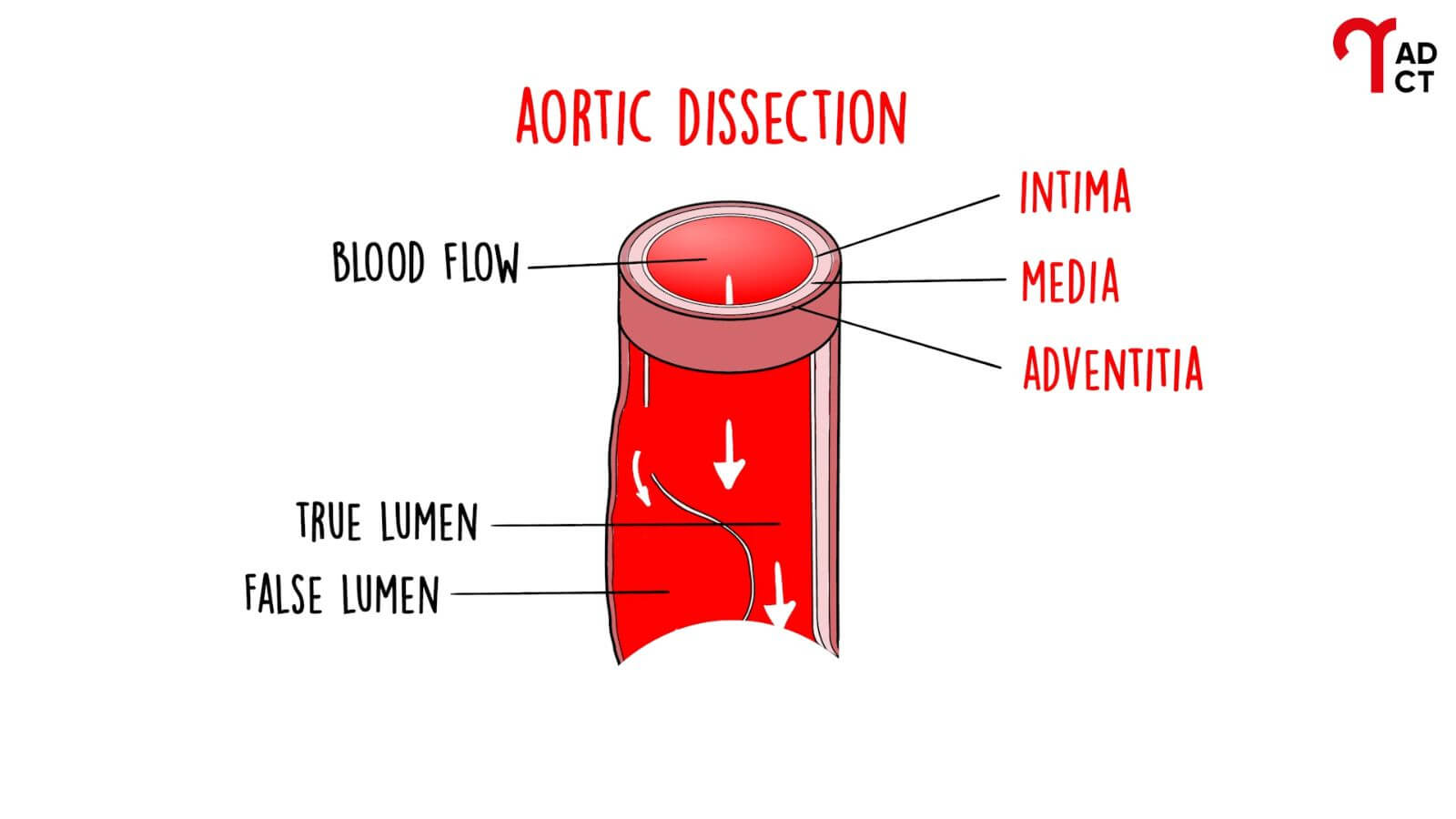
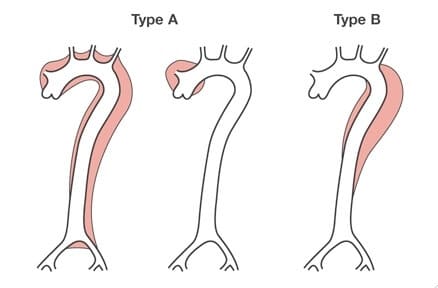
Aortic dissection is caused by a partial tear in the wall of the aorta. This tear then spreads along the length of the aorta. This can rupture or interrupt the blood supply to vital organs. If the tear occurs in the first part of the aorta, in the front of the chest, it is called a type A dissection. If it occurs in the aorta in the back of the chest, it is a type B dissection. In some cases, an aortic dissection can involve the aortic arch without extending to the ascending aorta. This is known as a non-A non-B dissection.
Aortic dissection can affect adults of any age. It is an important cause of maternal death. Untreated type A dissection is almost always fatal. Type B dissection is much less dangerous and is rarely fatal in the short term.
In the UK & Ireland, over 2,000 people per year lose their lives from aortic dissection, by contrast, 1,870 people per year lose their lives in road traffic accidents. Whilst death in pregnancy is very rare, 11% of maternal deaths from cardiovascular causes are due to aortic dissection. These numbers are projected to almost double by 2050. We are working on improving the future care of aortic patients.
Symptoms
Acute aortic dissection can present with a wide range of symptoms. The most common is the sudden onset of severe pain, typically felt in the chest, back, neck, or abdomen, or in a combination of these areas. This pain is usually maximal at the moment it begins. As the dissection progresses along the aorta, the pain may radiate to other parts of the body. Once stable blood flow is established within the aorta, the pain may subside, which can delay or obscure diagnosis.
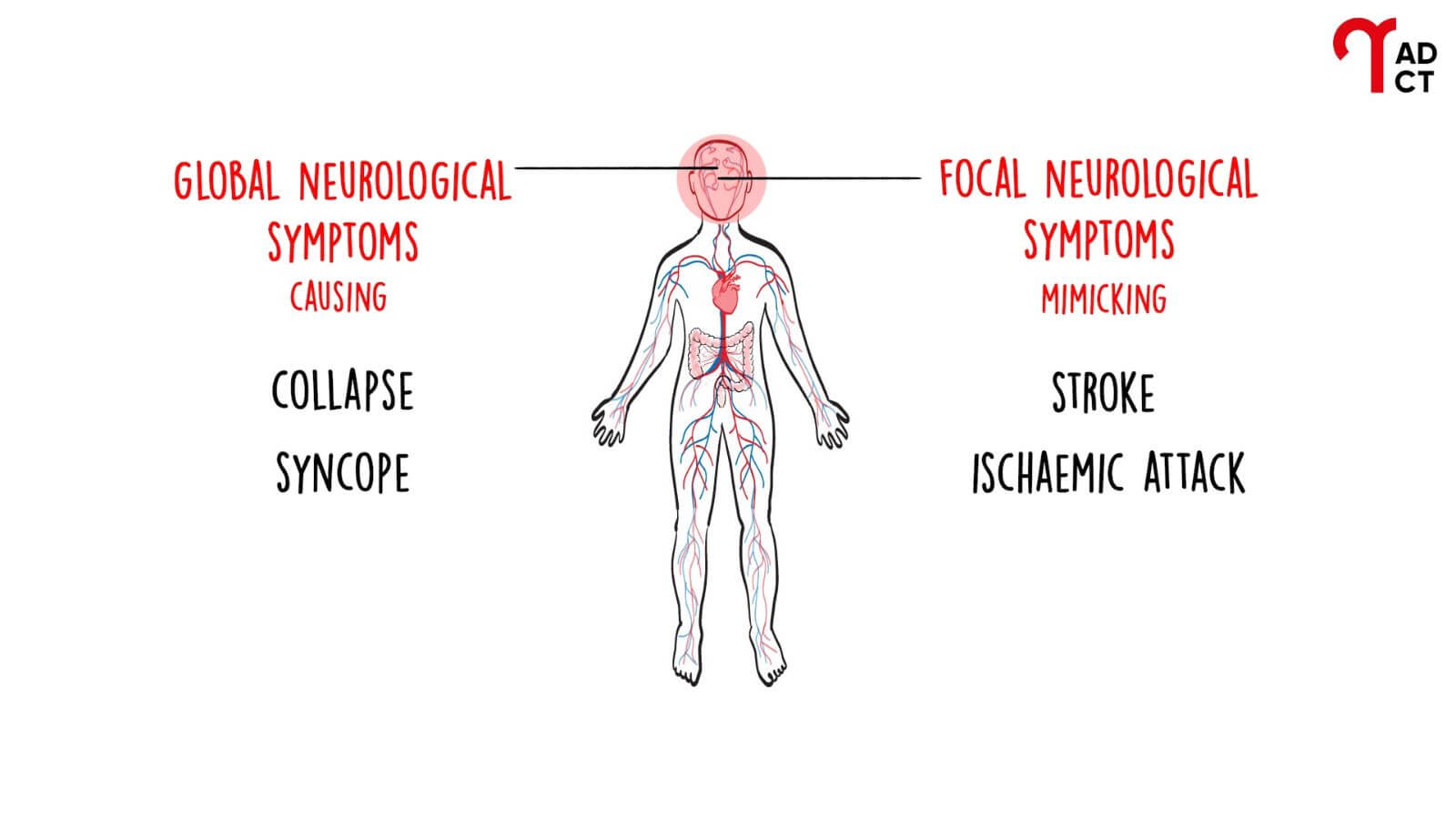
Unlike many other emergencies, aortic dissection does not always present with classic symptoms. Around one-third of patients are misdiagnosed because they may appear asymptomatic on arrival at the Emergency Department or display a complex mix of transient symptoms. These symptoms result from malperfusion (temporary disruptions in blood flow to different organs) caused by the dissection compressing the true lumen of the aorta.
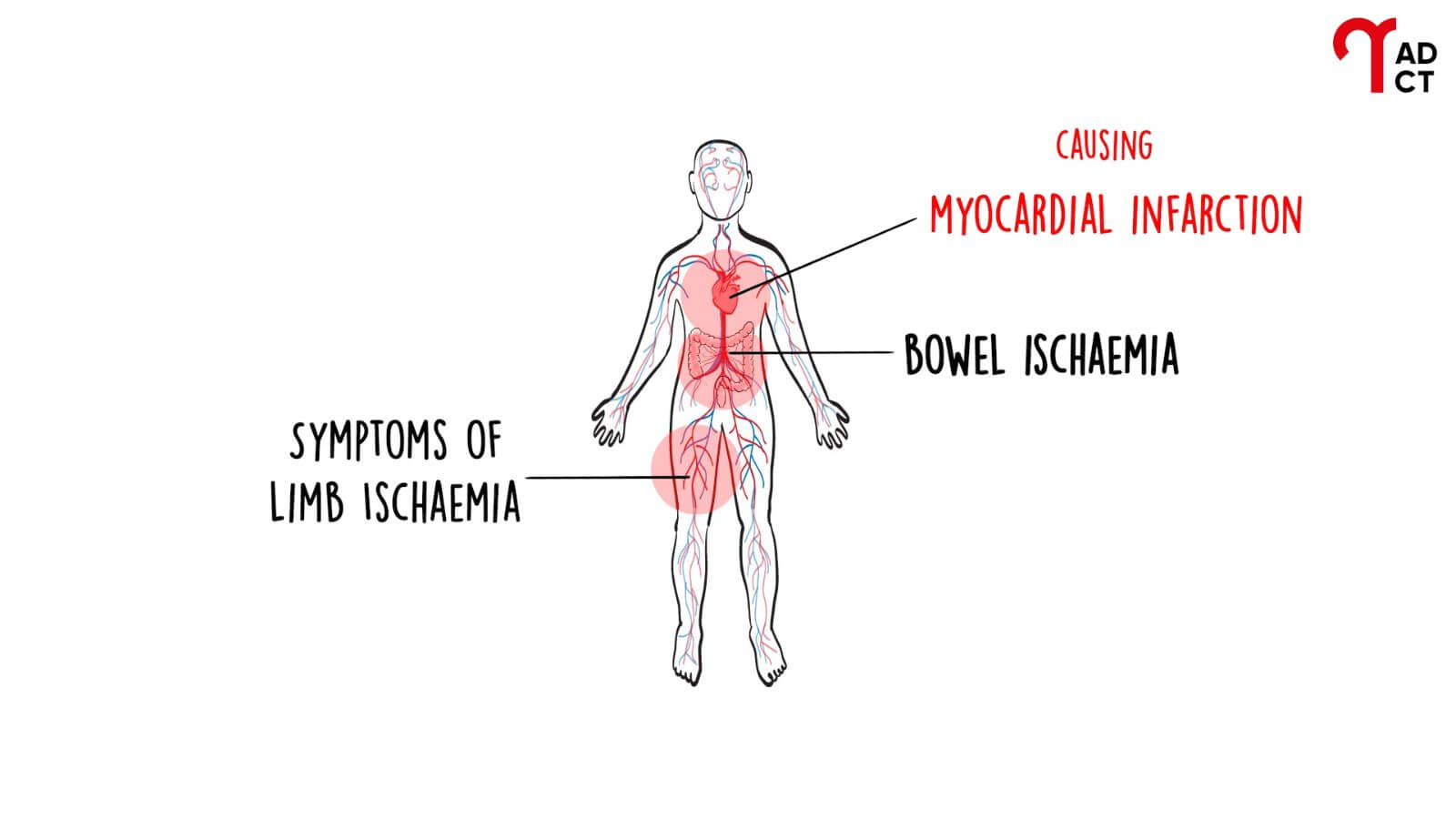
Depending on which arteries are affected, symptoms may vary. If the coronary arteries are involved, the patient may experience a heart attack. If cerebral blood flow is reduced, symptoms may include fainting, confusion, or stroke-like effects such as weakness or speech difficulties. Involvement of the mesenteric arteries can cause ischaemia (a reduction or complete loss of blood supply) of the bowel, while limb ischaemia may occur if blood supply to the arms or legs is compromised.
Understanding that aortic dissection can present in such diverse and non-specific ways is essential.
Risk Factors
Lifestyle
- Age-related aorta wear and tear
- Hypertension
- Atherosclerosis
- Smoking
- Cocaine use
- Weightlifting
- Pregnancy
- Blunt chest trauma
Genetic & connective tissue conditions
- Bicuspid aortic valve
- Congenital aortic stenosis
- Aortic aneurysm
- Family history of aortic dissection (ACTA2)
- Noonan syndrome
- Marfan syndrome
- Loeys-Dietz syndrome
- Meester-Loeys syndrome
- Cutis Laxa
- Arterial tortuosity syndrome
- Ehlers-Danlos syndromes
- Turner syndrome
- DiGeorge syndrome (22q11 deletion)
- Multisystemic Smooth Muscle Dysfunction Syndrome (MSMDS)
Autoimmune & Inflammatory conditions
- Giant Cell Arteritis & Polymyalgia Rheumatica
- Takayasu’s arteritis
- Polyarteritis nodosa
- Behçet’s disease
- Systemic lupus erythematosus
- Scleroderma
- Granulomatosis with polyangiitis
- Microscopic polyangiitis
- Sarcoidosis
Diagnosis
These people do not die because the NHS lacks the facilities to treat them. Cardiac surgical units across the country have the capacity to carry out the extra operations required. The problem is that people are not diagnosed quickly enough, if at all.
Patients with aortic dissection typically suffer sudden severe chest pain. The pain can settle completely and routine tests carried out in the Emergency Department can be normal. To make the diagnosis it is necessary to carry out an emergency CT scan. Too often a diagnosis of aortic dissection is not considered and a CT scan is not ordered at all.
Emergency Departments see many patients with chest pain and only a few will have an aortic dissection. However, we know that the number of CT scans performed increases greatly in Emergency Departments that ask the question ‘could it be aortic dissection?’ for all patients with chest pain, and as a result, no patients with an aortic dissection have the diagnosis missed.
33%
of those suffering from an aortic dissection are misdiagnosed
2000
people per year lose their lives from aortic dissection in the UK
11%
of maternal deaths from cardiovascular causes are due to aortic dissection
10
lives could be saved per week with the correct diagnosis
Treatment
Treatment for type A dissection requires emergency open-heart surgery. This will save the lives of over three-quarters of patients. Over 2800 patients per year suffer a type A dissection in the UK & Ireland (2,300 in England). Half of these die almost immediately after the onset. Although the number of operations for type A dissection is increasing, still only two-thirds of patients who could be saved undergo an operation. This means that over 500 people per year in the UK & Ireland (380 in England), or 10 people per week, could be saved.
Long-Term Care
Patients who survive an aortic dissection have a long-term condition that places them at risk of future complications. To minimise the risk of these complications developing and treat them effectively if they occur, patients need to be monitored by specialist medical teams, but the provision of this specialised monitoring for patients is variable. See more information and advice about living with aortic dissection.
Screening Relatives
Many conditions predispose a person to aortic dissection and some of these are inherited. If those relatives at risk are identified, measures can be taken to reduce their risk of developing aortic dissection. Whilst some of these genetic conditions are well known and easy to screen for, others are less well known and understood. Screening relatives for these conditions requires specialised clinical genetics input, and relatives’ access to these services is variable. Our patient resource, genetic testing for aortic dissection explains who should get diagnostic genetic testing, as well as the requirements for testing.
Patient Resources
Guiding you on your journey following an aortic dissection. Free online resources for families and those who have or are at risk of aortic dissection.
Primary Care Field Guide
Supporting multi-disciplinary teams of GPs, nurses, pharmacists & other healthcare professionals involved in cardiovascular disease care.
Frequently Asked Questions
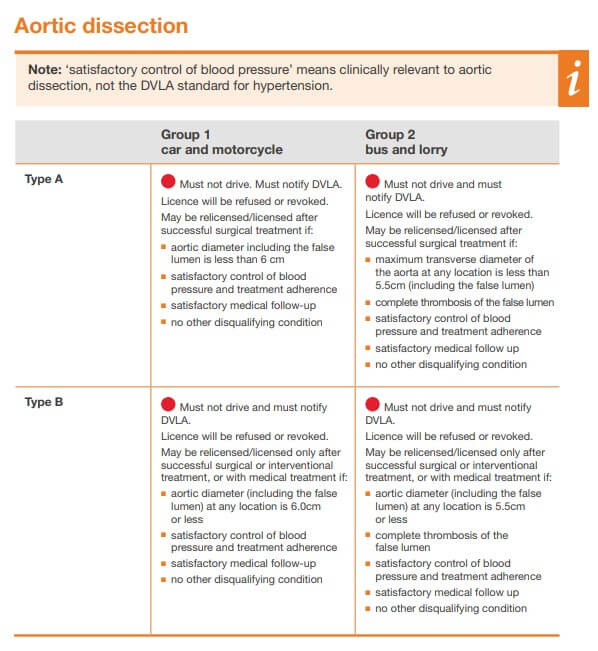
Driving After an Aortic Dissection
-
When can I resume driving after an aortic dissection?
You should seek advice from your medical team regarding when to resume driving after an aortic dissection. Typically, if you have undergone surgery, you will be advised not to drive for up to 6 weeks post-operation. It’s crucial to ensure that you are fully healed and can be in complete control of a vehicle, with the ability to perform an emergency stop safely.
-
Do I need to notify the DVLA about my aortic dissection?
Yes, the DVLA has specific rules concerning individuals affected by certain medical conditions, including aortic dissection. You must inform the DVLA, as you could be fined for failing to report your condition. The rules are more stringent for professional drivers.
Anyone who has experienced an aortic dissection, whether type A or type B, with or without surgery, and with or without complications, should notify the DVLA by completing the Report your Medical Condition H1 form. With a change in the DVLA rules in 2020, those who have experienced aortic dissection in the past are required to inform the DVLA. While awaiting the outcome of the notification, you may continue to drive unless your medical team advises otherwise.
Full information regarding medical conditions and driving can be found on the DVLA website at www.gov.uk/health-conditions-and-driving. It’s important to check this resource for the most up-to-date guidelines. -
Should I inform my car insurance provider about my aortic dissection?
Yes, it’s essential to notify your insurance company about your aortic dissection to ensure that your coverage remains valid.
-
Am I required to wear a seatbelt if I've had an aortic dissection?
Yes, even after an aortic dissection and surgery, you are not exempt from wearing a seatbelt. For comfort, you may place a folded towel between the seatbelt and your chest to reduce pressure on the area of surgery.
-
What are the DVLA guidelines for driving after a type A dissection?
For a type A dissection, you must not drive and are required to notify the DVLA. Your licence will be refused or revoked, but you may be relicensed after successful surgical treatment, provided certain conditions are met, including an aortic diameter less than 6 cm, satisfactory blood pressure control, adherence to treatment, satisfactory medical follow-up, and no other disqualifying conditions.
Please note that ‘satisfactory control of blood pressure’ is measured with criteria that are clinically relevant to aortic dissection, not just the standard DVLA requirements for hypertension.
-
What are the DVLA guidelines for driving after a type B dissection?
Similar to type A, you must not drive after a type B dissection and must inform the DVLA. Relicensing may occur only after successful surgical or interventional treatment, or with medical management if the aortic diameter is 6.0 cm or less, among other conditions, including satisfactory blood pressure control specific to aortic dissection.
Please note that ‘satisfactory control of blood pressure’ is measured with criteria that are clinically relevant to aortic dissection, not just the standard DVLA requirements for hypertension.
-
Are the driving assessments different for bus and lorry licenses after an aortic dissection?
Yes, the assessments for professional driving licenses such as for buses and lorries are different and have their own set of guidelines. It is important to consult the DVLA for specific regulations related to professional licenses.
Please note that ‘satisfactory control of blood pressure’ is measured with criteria that are clinically relevant to aortic dissection, not just the standard DVLA requirements for hypertension.
Genetics
-
Is aortic dissection hereditary?
Acute aortic dissection is a medical condition that must be taken seriously, as it can quickly become life-threatening. While aortic dissection can happen to anyone, in about a third of patients it can be hereditary. It is especially important for people with a family history of aortic dissection to be aware of the potential risk. The good news is that if you have had an aortic dissection or have a relative who has suffered an aortic dissection, your doctor can refer you for genetic testing if appropriate.
-
What are the NHS criteria for genetic testing and screening for thoracic aortic aneurysms and dissections?
The NHS has established specific criteria to identify individuals who should be considered for genetic testing and screening for thoracic aortic aneurysms and dissections. These criteria are designed to target those at higher risk due to personal or family medical history. You or a family member may be eligible for testing if any of the following apply:
- Early Onset: A thoracic aortic aneurysm or dissection presenting before the age of 50.
- Family History with Early Onset: A thoracic aortic aneurysm or dissection presenting before the age of 60, in conjunction with a first-degree relative who has also had an aortic aneurysm or dissection.
- Early Onset without Cardiovascular Risk Factors: A thoracic aortic aneurysm or dissection presenting before age 60, in the absence of classic cardiovascular risk factors.
- Signs of Aortopathy: A thoracic aortic aneurysm or dissection presenting before the age of 60, with features suggestive of aortopathy, such as arterial tortuosity.
- Indications of Loeys-Dietz Syndrome: Clinical features strongly suggesting Loeys-Dietz syndrome.
- Marfan Syndrome Presentation: Features consistent with Marfan syndrome resulting in a systemic Ghent score of ≥7, after evaluation by a clinical geneticist or aortopathy specialist.
- High Clinical Suspicion: A strong clinical suspicion of a genetic predisposition to aortic or arterial disease, particularly when tests for conditions like Ehlers-Danlos syndrome have not found a causative mutation.
- Post-Mortem Consideration: Any individual who had a thoracic aortic aneurysm or dissection that was discovered posthumously, who meets any of the aforementioned criteria, may be considered for post-mortem genetic testing to inform and benefit living relatives through cascade testing.
If you or someone you know meets any of the above criteria, it is advised to consult with a GP or healthcare professional about the possibility of genetic testing and screening.
For the most current information and detailed guidance on genetic testing for familial aortic dissection, please refer to the National Genomic Test Directory. You can find the latest versions, including information on test R125 for Familial Aortic Dissection, at National Genomic Test Directories.
Diagnosis
-
How do you rule out an aortic dissection?
An aortic dissection can quickly become a deadly medical emergency, making a thorough and accurate diagnosis critical to a patient’s chances of recovery. If a doctor suspects a patient has an aortic dissection, confirmatory testing is needed in order to make a definitive diagnosis. A computed tomography (CT) scan is the reliable way of diagnosing or excluding an aortic dissection. With the right diagnosis, prompt treatment can be initiated, and a patient’s life saved.
-
Can aortic dissection be seen on xray?
Aortic dissection cannot be reliably seen on a simple x-ray. In most cases, aortic dissection is diagnosed using a computed tomography (CT) scan. This scan provides more detailed images of the aorta and can help doctors confirm the diagnosis of aortic dissection.
-
Can high blood pressure cause aortic dissection?
High blood pressure is an important cause of aortic dissection, and to reduce the risks of complications, it is extremely important that high blood pressure is well controlled. In the acute phase of an aortic dissection, blood pressure may be normal, elevated, or reduced. Treatment for acute aortic dissection will take into account a patient’s blood pressure.
-
What is aortic dissection type B?
Aortic dissection type B, also known as Stanford type B aortic dissection, is a type of aortic dissection that affects the descending aorta. Located in the back and carrying blood down to the abdomen and legs.
-
What is aortic dissection type A?
Aortic dissection type A, also known as Stanford type A aortic dissection, is a type of aortic dissection that affects the ascending aorta, which is the part of the aorta that carries blood from the heart up towards the arms and the brain.
-
Why a blood pressure difference between arms?
A difference in blood pressure between the arms can be a sign of aortic dissection, although it is only present in about 15% of patients with an aortic dissection. So, if there is no difference in blood pressure between the arms this does not allow an aortic dissection to be ruled out. Aortic dissection is a serious condition that involves a tear in the inner layer of the aorta, the large blood vessel that carries blood from the heart to the rest of the body. This tear can cause blood to flow between the layers of the aortic wall, leading to the formation of a false lumen, or channel.
In some cases, the difference in pressure between the false lumen and the true lumen can affect blood flow to the arms. If the pressure in the false lumen is higher than the pressure in the true lumen, it can cause the blood vessels in the arms to become compressed, reducing blood flow and leading to a lower blood pressure in the affected arm.
-
Is a cardiac stress test useful for aortic dissection?
A cardiac stress test is not useful in the diagnosis of acute aortic dissection and may well be dangerous. A cardiac stress test is a test that is used to evaluate how well the heart is functioning during physical activity. It may be helpful in the long term stage of aortic dissection in helping assess the risk of a surgical intervention.
-
What is the most common cause of aortic dissection?
The most common cause of aortic dissections is high blood pressure. Other possible causes of aortic dissections include a congenital heart defect, certain infections, connective tissue disorders, such as Marfan syndrome or Ehlers-Danlos syndrome, a trauma-related injury to the aorta, and drug abuse.
Even though these potential causes may appear to be unrelated, seeking out medical help for a suspected or diagnosed aortic dissection is necessary for receiving the proper care and treatment needed from a specialist doctor.
-
When should you suspect an aortic dissection?
There are a few key signs to look out for that can indicate a potential aortic dissection before it becomes more serious. Sudden, severe chest or back pain that does not go away after a few moments, sweating, dizziness, or shortness of breath are all symptoms of aortic dissection, and you should seek immediate medical attention. Prompt diagnosis and treatment are important for improved patient outcomes.
Patient Experiences
-
What does aortic dissection feel like?
An acute aortic dissection can present with many symptoms and can be a frightening experience. Most people with aortic dissection describe severe chest pain, that may radiate through to the back and may even extend to the abdomen and neck area. The onset of the pain is sudden, and the pain is usually most severe initially. The sheer intensity of the pain during aortic dissection often causes a feeling of serious panic and fear. While aortic dissection can be a very frightening experience, it is important to note that with early diagnosis and timely treatment, most cases are able to have successful recoveries.
-
Is aortic dissection painful?
An acute aortic dissection can present with many symptoms and can be a frightening experience. Most people with aortic dissection describe severe chest pain, that may radiate through to the back and may even extend to the abdomen and neck area. The onset of the pain is sudden, and the pain is usually most severe initially. The sheer intensity of the pain during aortic dissection often causes a feeling of serious panic and fear. While aortic dissection can be a very frightening experience, it is important to note that with early diagnosis and timely treatment, most cases are able to have successful recoveries.
-
Can aortic dissection pain come and go?
Yes, aortic dissection pain can come and go. Aortic dissection is a serious condition in which the inner layer of the aorta, the large blood vessel that carries blood from the heart to the rest of the body, tears. This can cause severe chest or back pain that may come and go or be constant. It is important to seek medical attention immediately if you think you may be experiencing symptoms of an aortic dissection. This condition can be life-threatening if not treated promptly.
-
Is aortic dissection pain constant?
Many people experience extreme aortic dissection pain, but it doesn’t necessarily remain constant. It can come on suddenly and then subside, or even stop altogether. It is important to remember that chest pain of any kind should not be ignored, so if you experience aortic dissection pain – whether it’s constant or episodic – don’t hesitate to see a doctor for a professional diagnosis.
-
How long can an aortic dissection last?
The symptoms associated with an acute aortic dissection may last hours or days. After treatment, the majority of patients are left with a portion of their aorta that is dissected. It is important that this is monitored with regular scans and with advice on how to manage an aortic dissection.
-
Is aortic dissection a heart attack?
Aortic dissection and a heart attack are different medical emergencies. Both usually present with chest pain, but the nature of this pain is usually different. A heart attack can be diagnosed with a combination of a blood test and an ECG (heart tracing) but aortic dissection requires a CT scan to make a diagnosis. Not only are aortic dissection and heart attack two distinct conditions, they also have different treatments. Understanding the difference between an aortic dissection and a heart attack can be crucial to ensuring the best outcome for those affected by either condition.
-
Which type of aortic dissection is worse?
Aortic dissection is a serious, life-threatening condition that requires prompt medical attention. The two primary types of aortic dissection are Stanford type A and Stanford type B. While both require urgent treatment, a Stanford A aortic dissection is considered more severe than a Stanford B aortic dissection. It is more likely to be fatal if not promptly treated.
Treatment
-
Can aortic dissection be cured?
While aortic dissection cannot be cured, there are treatments available that can help manage symptoms and limit complications from the condition. Depending upon the type and severity of aortic dissection, treatment can range from lifestyle changes or medications to surgery or a combination of interventions. The good news is that aortic dissection can be successfully treated in a way that gives patients a better quality of life if they get a correct diagnosis and get medical help right away.
-
Can aortic dissection heal itself?
Very minor forms of aortic dissection may heal themselves on their own in certain cases. This, however, is very uncommon. In most cases, if the aortic dissection is very extensive, some form of intervention will be required to repair it.
-
How long will I be in the hospital after aortic surgery?
After a typical aortic dissection surgery, a person can generally expect their hospital stay to be approximately two weeks, though times may vary depending on individual factors. Each aortic surgery is unique and can take anywhere from a few days up to a month, depending on the extent of the procedure. Factors that affect a person’s hospital stay include age, pre-existing medical conditions, type of aortic dissection surgery performed, and post-operative recovery process.
After leaving the hospital, some people experience a lengthy period of home convalescence before fully recovering from the intrusive procedure. The duration of the recovery process varies per individual and depends on adherence to medical advice and protocols given by care providers. No matter the length of a person’s hospital or home recovery time after aortic surgery, it is best to relax, remain patient, follow all doctor’s orders carefully, and get outside help as needed in order to ensure an expeditious and successful recovery process.
-
What are the most effective medicines for aortic dissection?
The most effective treatment for aortic dissection is prompt medical care. This typically involves medications to control the heart rate and blood pressure, as well as surgery to repair the damaged aorta. Some of the medications that may be used to treat aortic dissection include beta blockers, calcium channel blockers, and ACE inhibitors. These medications are typically given to help control the heart rate and blood pressure and to prevent further tearing of the aorta. It is important to follow the treatment plan recommended by your doctor in order to prevent complications and improve your chances of a successful recovery.
-
How is aortic dissection repaired?
For acute aortic dissection, this depends on the location of the aortic dissection. If type A, repairs usually require open heart surgery. If type B, no repair may be necessary, if it is, this is usually done with a stent inserted through the groin. Recovery from aortic dissection repair surgery can take several weeks or longer, depending on the extent of the surgery and the patient’s overall health. It is important for patients to follow their doctor’s instructions for post-operative care, including taking medications as prescribed and attending follow-up appointments.
-
Why Esmolol for aortic dissection?
In acute aortic dissection, it is important to control blood pressure. Esmolol is one drug that can be given intravenously to rapidly control blood pressure. Labetalol is another similar drug that is sometimes used. Esmolol and Labetalol both work by reducing the rate at which the heart contracts and the force of that contraction, thus reducing blood pressure. Labetalol also acts on receptors throughout the body to reduce blood pressure.
-
How do stents work for aortic dissection?
Stents are small metal mesh tubes that are used to support narrowed or weakened blood vessels. In the case of aortic dissection, a stent may be used to help keep the aorta open and prevent it from tearing further. A stent is typically inserted using a catheter, a thin, flexible tube that is inserted into a blood vessel through a small incision in the groin. The stent is then carefully positioned at the site of the dissection and expanded to support the aorta. This helps to keep the aorta open and prevent further tearing, allowing blood to flow more freely. Stenting is typically used in combination with other treatments, such as medications and surgery, to treat aortic dissection.
-
What is branched & fenestrated repair in aortic surgery?
Branched and fenestrated repair is a type of surgery used to repair the aorta in patients with complex aortic aneurysms or dissections. In this type of surgery, a custom-made stent graft is used to repair the aorta. The stent graft has branches and fenestrations, or openings, that allow blood to continue flowing to the side branches of the aorta, such as the iliac and renal arteries. This type of repair can be performed using minimally invasive techniques, which can reduce the risk of complications and speed up the recovery process. It is an alternative to open surgery, which involves making a large incision in the chest or abdomen to repair the aorta. Branched and fenestrated repair can be an effective treatment option for patients with complex aortic aneurysms or dissections.
-
Can aortic surgery affect vision?
Very rarely an acute aortic dissection may affect vision by interfering with blood flow to the brain. Visual impairment is also a potential, albeit very rare, complication of some forms of surgery for aortic dissection.
Living with Aortic Dissection
-
What activities should I avoid if I have an aortic dissection?
You should avoid any activity that may increase your blood pressure or strain on your heart. This includes activities that involve heavy pushing, pulling, bearing down, or lifting. Additionally, you should avoid shovelling snow, chopping wood, digging earth, or using a sledgehammer. Participating in rigorous, competitive or contact sports, and going on high-adrenaline amusement park rides.
-
How long can you live with an aortic dissection?
The length of time that a person can live with an aortic dissection depends on a variety of factors, including the type and location of the dissection, the presence of any other underlying medical conditions, and the person’s age and overall health. In some cases, aortic dissection can be treated successfully, and the person can live a normal lifespan. In other cases, aortic dissection can be life-threatening, and the person may die within days or even hours of the onset of symptoms.
If an acute aortic dissection is diagnosed and treated promptly, the chances of survival are generally good. However, aortic dissection is a lifelong condition, and a proportion of patients will have complications in the future.
-
How common is aortic dissection?
Aortic dissection is a relatively rare condition, with an estimated incidence of 6 cases per 100,000 people per year. It is more common in men than in women, and it is more likely to occur in older adults, with the majority of cases occurring in people over the age of 65. However, it is important to know that aortic dissection isn’t exclusive to these groups of people, and in fact, anyone at any age can suffer from the condition.
-
Is aortic dissection fatal?
Aortic dissection is a life-threatening condition that can be fatal if not treated quickly. Fortunately, aortic dissection can be diagnosed early, and with strong support from a medical team, the prognosis for a successful recovery can be much brighter. Although aortic dissection is a serious and potentially fatal health issue, a diagnosis does not necessarily mean a bad outcome. In many cases, treatments are effective in reducing complications and helping prevent a fatal outcome.
-
Does my family need to be screened for aortic dissection?
It’s a good idea for all families to assess the risk of aortic dissection. It can be a life-threatening condition, but fortunately, it’s also one that can often be successfully treated if caught early enough. Knowing your family history can help you determine your own risk level, so get together with your family members and go through any records you have regarding health and medical issues related to aortic dissection. The more information you have on hand, the easier it will be to put together a plan for monitoring this potential danger in the future.
-
Does aortic dissection qualify for disability?
Aortic dissection is a very serious condition that can require a lot of medical care. It can be a debilitating illness, and its symptoms can cause a great deal of pain and difficulty with day-to-day activities. That is why it is so important to be aware that aortic dissection may qualify for Universal Credit, Personal Independence Payment (PIP) or Disability Living Allowance (DLA). Depending on the individual case, a person with aortic dissection might be eligible for a financial allowance to help cover the costs associated with the medical care they need as well as lost earnings due to being unable to work.
However, eligibility will depend on each case and is determined by various criteria, so if you or a loved one is dealing with an aortic dissection, it’s important to contact a professional and inquire about what this could mean for you or your family member.
-
How to prevent aortic dissection?
Those at a higher risk of aortic dissection should be particularly aware of the signs, symptoms and preventative measures needed. Knowing the risk factors associated with aortic dissection is always a good starting point – high blood pressure, a family history of aortic diseases, connective tissue disorders, bicuspid aortic valves, and physical exertion can all increase the likelihood of an aortic dissection event. Seeking regular preventive care from your doctor is an essential step in preventing an aortic dissection from happening, along with monitoring your blood pressure levels throughout the day and making lifestyle changes to address any underlying causes that may result in hypertension – such as losing weight and increasing physical activity levels.
Taking these simple precautionary steps can make all the difference in preventing an aortic dissection. For some patients with a hereditary cause of aortic dissection, surgery may be advised to prevent the occurrence of an aortic dissection.
-
Why is it important to take antibiotics before dental or invasive procedures if I've had a surgical repair of my aortic dissection?
Taking antibiotics before dental or invasive procedures is crucial for individuals who have had a surgical repair of their aortic aneurysm or dissection. This is because these procedures can introduce bacteria into the bloodstream, which can cause an infection around the aorta. It is important to talk to your aortic specialist before having any dental work.
-
What antibiotics should I avoid if I have aortic dissection?
Fluoroquinolone antibiotics such as Cipro (ciprofloxacin), Levaquin (levofloxacin), Factive (gemifloxacin), and Avelox (moxifloxacin) should be avoided if you have aortic dissection. These medications may increase the risk of aortic dissections or ruptures. It’s important to discuss alternative medications with your doctor.
-
Can I exercise after having an aortic dissection?
Exercising regularly is a great way to stay active and live a healthier life, so it’s only natural that you would want to continue your routine after having an aortic dissection. The good news is that exercising after an aortic dissection is encouraged, provided it is light to moderate in intensity. It’s important to take your time and follow the advice of your doctor – they can help you determine a safe and effective exercise routine that won’t put too much strain on your aorta. Stretching and slowly increasing the intensity of your exercises over time is a great way to gradually strengthen your body after an aortic dissection.
-
What is the best diet for lowering or maintaining good blood pressure?
Maintaining a healthy diet to manage your low blood pressure can be a great way to stay on top of your health overall. Eating a balanced meal containing a combination of proteins and carbohydrates is a good place to start. Make sure you include plenty of fruits, vegetables, and whole grains in your diet as well. Additionally, limiting or avoiding any high-sodium foods is key to managing a lower blood pressure level.
For those with aortic dissection, doctors may recommend a specific diet plan tailored to their needs; this should always be followed as a precautionary measure to prevent further complications. Ultimately, forming a nutritious eating pattern according to your medical needs can help you maintain a healthy lifestyle while living with low blood pressure.
-
How long does an aortic stent last?
The lifespan of an aortic stent can vary depending on a number of factors, such as the patient’s overall health and the specific type of stent used. In general, however, aortic stents are designed to be long-lasting and may remain in place for many years, even a lifetime. If a stent does cause problems, it may need to be replaced or removed. It is important that the stent is checked as part of a routine checkup.
-
What are the routine checks for monitoring aortic dissection recovery?
Following aortic dissection, a crucial part of a patient’s recovery is ongoing monitoring. This will involve a regular scan to monitor the aorta. Working with an aortic specialist to build a personalised recovery plan that accounts for any risk factors can help ensure the best possible outcome. Focusing on a check-up schedule can be a great way to stay on top of aortic dissection recovery progress and feel reassured that all the right steps are in place. Through advocacy and open communication with medical professionals, it is possible to enjoy a full recovery post-aortic dissection.
-
What kind of physical activity is safe for me if I have aortic dissection?
Mild to moderate physical activity is safe for patients with aortic dissection. Activities such as walking, biking, swimming, dancing, light jogging or stair climbing are good options when living with aortic dissection. However, it’s important to consult your doctor before starting any exercise regimen.
-
Can I scuba dive after an aortic dissection?
It is not recommended for individuals who have had an aortic dissection to engage in activities such as scuba diving. After an aortic dissection, it is important to follow your doctor’s instructions for care and avoid activities that may put additional strain on the aorta or increase your risk of further dissection. Scuba diving can put a lot of pressure on the aorta and increase the risk of complications, such as aortic rupture or bleeding. It is important to talk to your doctor about any activities you are considering and to follow their recommendations for your care.
-
Can I have sex after aortic surgery?
It’s a common question after aortic surgery – can I have a normal sex life? Generally speaking, the answer is yes. However, it’s a good idea to first get the go-ahead from your surgeon given any aortic dissection that occurred during your surgery. Depending on the extent of the aortic dissection, a doctor will typically recommend refraining from sexual activities for 6-12 weeks as a precautionary measure against any potential complications. Oftentimes, you may be able to resume lighter activities before this point with approval from your physician. Remember to listen to your body and take things at a slow pace to allow for proper healing post-surgery!
-
Can I get a tattoo or body piercing if I have an aortic dissection?
It is not recommended to get a tattoo or body piercing if you have an aortic dissection. This is because these procedures carry a risk of infection, and is further complicated depending on the medication you have been prescribed.
-
My aortic valve was recently replaced, and I'm hearing a clicking sound. What exactly is it?
After aortic valve replacement, a clicking sound is a common complaint reported by patients. Generally, the noise is caused by a small disc that moves inside the artificial valve. While this sound may be alarming at first, it is often not a cause for concern as the disc typically remains in a single position and does not cause any damage to the aorta or heart. Most people become accustomed to the clicking. If you experience pain or irregular heartbeats with this clicking noise, it is recommended that you seek medical attention right away.
-
What can I do to keep my body at a healthy weight?
Keeping your body at a healthy weight is important for managing aortic dissection. You can achieve this by following a balanced diet and engaging in regular physical activity. Your doctor can guide you on a diet that is low in sodium, fat, and cholesterol.
-
Who has died from aortic dissection?
There are many famous people who have died from aortic dissection, including actors, musicians, and athletes. For example, John Ritter, the actor best known for his role on the TV show “Three’s Company,” died from aortic dissection in 2003. Others who died suddenly and unexpectedly from aortic dissections include Lucille Ball, Alan Thicke, playwright Jonathan Larson, diplomat Richard Holbrooke, Japanese actor Hiromi Tsuru, manga artist Kentaro Miura, and Depeche Mode keyboardist Andy Fletcher.
However, there have been notable survivors of this condition. While not an exhaustive list, some notable names include New Zealand cricketer Chris Cairns, Judas Priest guitarist Richie Faulkner, BBC radio presenter Bob Harris, and former English footballer Steve Perryman.
Related Conditions
-
Why does aortic dissection cause mediastinal widening?
Aortic dissection is a serious medical condition in which a tear has occurred in the aortic wall, causing blood to enter the wall of the aorta. This causes the aorta to expand and can give rise to mediastinal widening on a chest x-ray. This is not a reliable finding with which to diagnose aortic dissection however.
-
How should diabetic patients prevent aortic dissection?
Diabetic patients can take several steps to reduce their risk of aortic dissection. These may include:
- Managing blood sugar levels: It is important to regularly monitor blood sugar levels and to take steps to keep them within the target range. This may involve following a healthy diet, getting regular exercise, and taking medications as prescribed by your doctor.
- Controlling blood pressure: High blood pressure is a major risk factor for aortic dissection. Diabetic patients should work with their doctor to monitor their blood pressure and to take steps to keep it within the target range. This may involve making lifestyle changes, such as eating a healthy diet, getting regular exercise, and quitting smoking, as well as taking medications as prescribed.
- Avoiding tobacco: Smoking and other forms of tobacco use can damage the blood vessels and increase the risk of aortic dissection. Diabetic patients should avoid tobacco and secondhand smoke to reduce their risk.
- Managing other medical conditions: Diabetic patients may have other medical conditions, such as high cholesterol or heart disease. It is important to work with your doctor to manage these conditions and to take steps to reduce your risk.
By following these recommendations, diabetic patients can help reduce their risk of aortic dissection and improve their overall health. It is important to work with your doctor to develop a personalized plan for managing your diabetes and reducing your risk of aortic dissection.
-
Why does aortic dissection cause hypertension?
High blood pressure is an important cause of aortic dissection, and to reduce the risks of complications, it is extremely important that high blood pressure is well controlled.
Acute aortic dissection is a life-threatening condition that occurs when a tear in a major artery allows blood to flow between the layers of the artery wall. This can stimulate receptors in the wall of the aorta that cause blood pressure to be elevated. This hypertension can be dangerous as it places strain on the affected arterial wall and may cause further complications. However, if an aortic dissection is identified quickly and treated suitably with medication, then hypertension can be effectively managed over time and its devastating effects can be minimized. -
Is aortic dissection and aortic aneurysm the same?
Aortic dissection and aortic aneurysm are two different conditions. Aortic dissection is a medical emergency caused when a tear on the inside of the aorta causes blood to enter the wall of the aorta. An aortic aneurysm, on the other hand, is a bulge in the aorta caused by a weakening of the artery walls, which can rupture if left untreated. Both conditions are serious and require prompt medical attention. The best thing you can do is stay informed about your health so you can recognise any warning signs and get help as soon as possible if needed.
-
Can aortic dissection cause stroke?
Aortic dissection can cause a stroke due to a disruption of blood flow to the brain. Fortunately, prompt medical attention from a doctor can help increase the chances of a positive prognosis. It is important for individuals who are experiencing severe chest pain or difficulty breathing to seek medical care right away, as these are warning signs of a possible aortic dissection. With treatment, a patient has a much greater chance of recovery and avoiding any long-term complications such as stroke.
-
Can aortic dissection cause pericardial effusion?
Yes, aortic dissection can cause pericardial effusion. Pericardial effusion is a condition in which there is an abnormal accumulation of fluid in the pericardium, the sac that surrounds the heart. There are a wide range of other conditions that can cause pericardial effusion, however. In some cases, pericardial effusion can cause difficulty breathing and be life-threatening if not treated promptly.
-
How does aortic dissection cause cardiac tamponade?
Pericardial effusion is a condition in which there is an abnormal accumulation of fluid in the pericardium, the sac that surrounds the heart. If this accumulation of fluid is great enough, it can impair the function of the heart, and this is called cardiac tamponade. If aortic dissection causes a pericardial effusion, it is usually due to blood leaking from the wall of the aorta into the pericardium. This can rapidly progress to cause cardiac tamponade. Prompt treatment can relieve this.
-
How does aortic dissection cause pleural effusion?
Pleural effusion is an accumulation of fluid between the chest wall and the lung. There are many possible causes, but in aortic dissection, a pleural effusion may be caused by blood leaking from the aorta.
-
Why does aortic dissection cause kidney failure?
An aortic dissection is a medical emergency caused by a tear in the aorta. The aorta is a major artery responsible for carrying oxygenated blood from the heart to the rest of the body. When this tear occurs, it can cut off the blood supply to vital organs, such as the kidneys. As a result, kidney failure may occur due to a lack of fresh oxygen-rich blood flow. Fortunately, early detection and treatment can help minimize its effects and may prevent permanent damage.
References
- Howard DPJ, Banerjee A, Fairhead JF et al. Population-Based Study of Incidence and Outcome of Acute Aortic Dissection and Premorbid Risk Factor Control. 10-Year Results From the Oxford Vascular Study. Circulation. 2013;127:2031-2037
- Sullivan PR, Wolfson AB, Leckey RD, Burke JL. Diagnosis of acute thoracic aortic dissection in the emergency department. The American Journal of Emergency Medicine 2000;18:46-50.
- Zhan S, Hong S, Shan-shan L. Misdiagnosis of Aortic Dissection: Experience of 361 Patients. The Journal of Clinical Hypertension 2012;14:256-260
- Bottle A, Mariscalco G, Shaw MA et al. Unwarranted Variation in the Quality of Care for Patients With Diseases of the Thoracic Aorta. J Am Heart Assoc. 2017;6:e004913
-
Howard DP, Sideso E, Handa A, Rothwell PM. Incidence, risk factors, outcome and projected future burden of acute aortic dissection. Ann Cardiothorac Surg 2014;3:278-284
-
Knight M, Nair M, Tuffnell D, Kenyon S, Shakespeare J, Brocklehurst P, Kurinczuk JJ (Eds.) on behalf of MBRRACE-UK. Saving Lives, Improving Mothers’ Care – Surveillance of maternal deaths in the UK 2012-14 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-14. Oxford: National Perinatal Epidemiology Unit, University of Oxford 2016.
How you can help
We are always searching for volunteers to help out at our charity. Learn how you can support and become involved with The Aortic Dissection Charitable Trust.


Privacy Policy | Accessibility
The Aortic Dissection Charitable Trust
Registered charity in England & Wales No. 1191420
Registered charity in Scotland No. SC051517
PO Box 812, Hope Valley, Chesterfield S40 9QY
The information and materials on this site are for general information purposes only. This site is not designed to provide individual medical advice, diagnosis or treatment. If you have any concerns, please speak to your GP. If you believe you have a medical emergency, call 999 immediately.