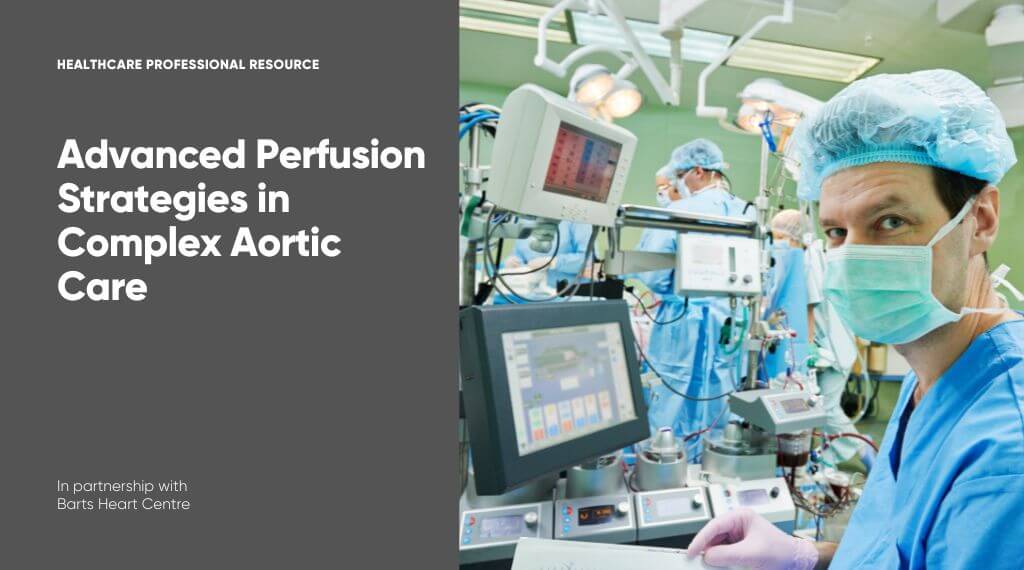
Barts Heart Centre, in collaboration with The Aortic Dissection Charitable Trust, hosted the second webinar in the AortaEd series on perfusion management for aortic dissection. This event, Innovations in Perfusion for Aortic Dissection: Circuitry, Techniques, and Complex Case Management, provided an in-depth exploration of cutting-edge technologies and strategies used to manage the complexities of aortic dissection. Leading experts across multiple disciplines shared their insights, with a strong focus on improving patient outcomes through innovation, teamwork, and precise perfusion strategies.
Perioperative Management: Prevention and Early Detection of End-Organ Damage
Dr Carlos Corredor Rosero, Consultant in Cardiothoracic Anaesthesia and Intensive Care at St Bartholomew’s Hospital, opened the session by discussing the critical aspects of perioperative management in acute aortic dissection. A life-threatening condition, aortic dissection requires swift, specialised intervention to prevent devastating complications such as organ failure, neurological damage, or coronary dysfunction. Dr Corredor emphasised blood pressure control, pain management, and timely surgical intervention as key pillars of treatment. He also highlighted advanced monitoring techniques such as transoesophageal echocardiography (TOE) and near-infrared spectroscopy (NIRS) to ensure adequate brain and organ perfusion during surgery. Post-operatively, the multidisciplinary team focuses on protecting vital organs and managing complications like coagulopathy, all while maintaining anaesthetic stability during critical phases of surgery.
Advanced Circuitry and Haemofiltration
Cristina Revilla Martin, Senior Clinical Perfusionist at St Bartholomew’s Hospital, introduced attendees to the intricate role of heart-lung machine circuitry and haemofiltration in perfusion management for aortic dissection surgeries. Cristina discussed the importance of optimising the cardiopulmonary bypass (CPB) circuit, particularly when cerebral perfusion is involved. She presented the benefits of centrifugal pumps, which self-regulate blood flow, and detailed the use of haemofiltration and Cytosorb filters to manage fluid balance and reduce inflammation. Advanced flow monitoring tools are crucial in tracking perfusion accuracy, while cerebral oximetry ensures brain safety by detecting hypoxia early.
Optimising Myocardial Preservation with Custodial HTK
Derek Wiggins, Lead Clinical Perfusionist, explored myocardial preservation techniques during aortic dissection repair. He discussed the shift from traditional blood cardioplegia to custodial HTK solution, which allows surgeons to operate for longer without needing to re-dose, crucial during lengthy and complex procedures. By inducing diastolic arrest with minimal ionic disturbance, custodial HTK provides protection for up to 90 minutes. However, Derek warned of the challenges related to fluid overload and sodium depletion, which require careful management through haemofiltration or cannulation strategies. Ensuring fluid balance and electrolyte stability are essential to safeguarding the heart during surgery.
Innovations in CPB Monitoring
Bruno Claro, Lead Clinical Perfusionist for Education at Barts Heart Centre, took a forward-looking approach, discussing advances in cardiopulmonary bypass (CPB) monitoring. His focus was on real-time monitoring techniques, which help detect perfusion issues early, ensuring patient safety. Bruno detailed the use of tools such as infrared spectrometry (NIRS) and cerebral pressure monitoring, critical in maintaining optimal brain perfusion during complex surgeries. These techniques become particularly important during deep hypothermic circulatory arrest (DHCA) or selective antegrade cerebral perfusion (SACP). He also introduced emerging technologies such as AI-driven monitoring systems, which hold promise for future advances in perfusion safety and outcomes.
Challenging Case Studies in Complex Aortic Surgery
Dani Blackie, Lead Perfusionist at Barts Heart Centre, presented a series of challenging case studies that underscored the complexity and variability of aortic dissection care. One case involved managing a patient with sickle cell trait, which posed a unique risk during bypass surgery. The team employed strategies like normothermia and high oxygenation to avoid sickle cell complications during aortic root replacement. Another case featured a lupus patient with acute dissection, requiring careful coagulation management due to the presence of antiphospholipid antibodies. The third case involved a Jehovah’s Witness patient, requiring creative approaches to avoid blood transfusions during emergency surgery. All three cases demonstrated the importance of tailoring perfusion strategies to the individual needs of the patient and the value of multidisciplinary collaboration.
Cytosorb Technology in Aortic Surgery
Pamela Leckie, an International Application Specialist from CytoSorbents Medical UK Ltd, highlighted the use of Cytosorb technology in cardiopulmonary bypass (CPB) circuits during aortic dissection surgery. Cytosorb acts as an adsorber, removing inflammatory mediators from the blood, thus helping to reduce the systemic inflammatory response that often accompanies complex surgeries. Pamela demonstrated how this technology can improve patient stability by reducing the need for blood transfusions, minimising ventilator hours, and preventing post-operative complications such as coagulopathy.
Neurological Protection and Flow Monitoring
Professor Aung Y Oo, Consultant Cardiac Surgeon and Clinical Lead for Aortovascular Surgery at Barts Heart Centre, provided insights into techniques for protecting the brain during aortic dissection surgeries. He explained the role of hypothermic circulatory arrest (HCA) and selective antegrade cerebral perfusion (SACP) in maintaining cerebral blood flow and preventing stroke. Real-time monitoring, including the use of cerebral oxygen saturation monitors and transcranial Doppler, was discussed as critical to ensuring brain perfusion. Professor Oo reinforced the importance of comprehensive preoperative planning and intraoperative precision to minimise the risk of neurological complications.
Coagulation Management in Aortic Dissection
Dr Martinette Ferriera closed the session with a comprehensive overview of coagulation management during aortic dissection surgery. She addressed the challenge of managing anticoagulated patients and those with coagulopathies due to the dissection process itself. Dr Ferriera highlighted the use of antifibrinolytic agents, such as tranexamic acid, to control bleeding, and the importance of viscoelastic testing to guide haemostatic interventions. She stressed that multidisciplinary collaboration and real-time coagulation monitoring are essential to successful surgical outcomes.
This webinar provided a rich and detailed look at the latest innovations in perfusion management for aortic dissection, offering both theoretical insights and practical applications. With a focus on teamwork, precision, and continuous learning, the experts at Barts Heart Centre delivered a comprehensive view of how cutting-edge techniques and technologies are transforming care for patients with complex aortic conditions.