This week, the charity contributed to the 2025 ACCESS Autumn Clinical Development Day in London. A day which brought together leading clinicians from across the capital, emergency physicians, anaesthetists, intensivists, paramedics and transfer teams. ACCESS, the Adult Critical Care Emergency Support Service, is now at the heart of critical care transfers in London. Improving outcomes for patients whose survival depends on rapid, coordinated care.
From Patient to Advocate
A powerful part of the day came when Valérie, a survivor of type A aortic dissection, shared her story on behalf of the charity. In 2019, Valérie went from healthy and active to critically ill in a matter of moments. Despite intense pain and neurological symptoms, her condition was not initially recognised and she was misdiagnosed. She suffered three strokes. And she was nearly lost to a condition that still too often slips under the radar.
Valérie reminded the room that behind every data point is a person who has been through trauma, or a family still grieving. Her story challenged clinicians to reflect not only on practice, but on communication, compassion and why the system must do better.

What is ACCESS?
ACCESS is London’s coordinated critical care transfer service. Since April 2023, it has provided a single point of access for adult patients who need urgent transfer between hospitals while on organ support. It is hosted by Barts Health NHS Trust, commissioned by NHS England (London), and delivered in partnership with the London Ambulance Service and London’s Operational Delivery Networks.
Its goal is to make critical care transfers safer, faster and more consistent. When patients like Valérie need to be moved urgently to a specialist centre, there is no room for delay or error. ACCESS provides dedicated teams, specialist vehicles and a streamlined transfer process. It is already improving coordination across the capital and is a model that others should follow.
Why This Matters for Aortic Dissection
Aortic dissection is not rare in impact. It is one of the most time-critical emergencies a hospital can face. Type A dissections require immediate diagnosis, rapid transfer and emergency surgery.
A national audit published in 2024 by ACTACC confirmed what we at the charity hear far too often
- Patients are misdiagnosed
- Transfers are delayed
- Communication between hospitals is inconsistent
- Monitoring during transfer is inadequate
- Some patients are given medications that actively worsen their chances
These are not isolated incidents. They are systemic problems with devastating consequences.
From Data to Action
At the charity, we do more than raise awareness. We press for structural change. We work with the NHS, researchers, clinicians and most importantly, patients and families to identify what needs to improve, and how.
We know education alone is not enough. We cannot expect busy clinicians to just “think” aortic dissection without giving them the tools, protocols and systems to back that up. Hospitals need structured diagnostic pathways. They need decision-making support. They need triage training and a culture that encourages second opinions, not punishes them.
At places like Hull Royal Infirmary, we’ve seen that these changes are possible. A simple bundle of improvements reduced time to CT and ensured 100% detection of cases. That is the kind of progress we need to see everywhere.
The Role of Ultrasound
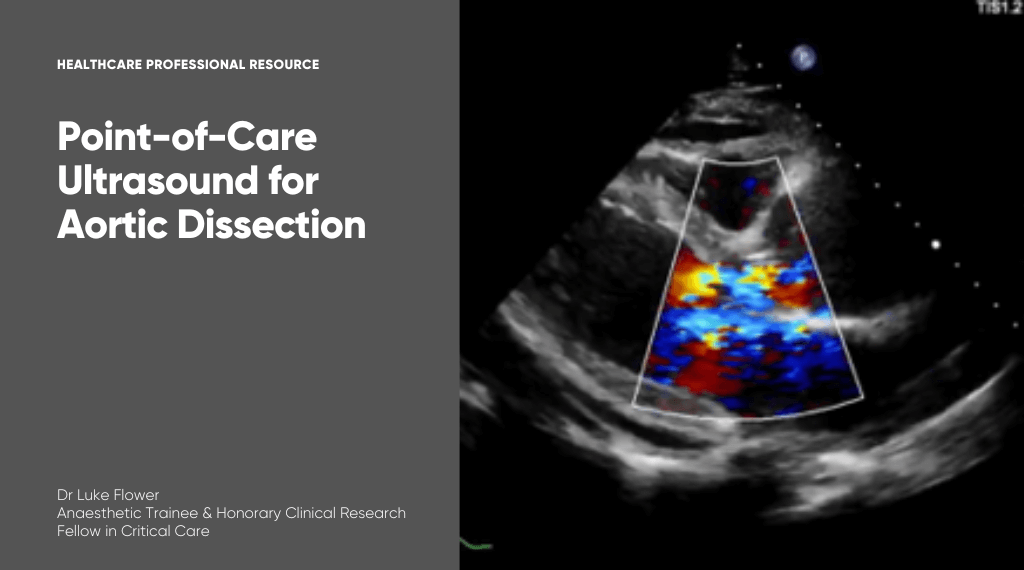
Dr Luke Flower also spoke at the Clinical Day, sharing his expertise on point-of-care ultrasound (POCUS) in the context of acute aortic syndromes. As an anaesthetic trainee and clinical research fellow in critical care, Luke demonstrated how ultrasound can support faster recognition of aortic dissection.
Luke’s presentation focused on the role of POCUS as a diagnostic aid in emergency and critical care settings. He highlighted its potential to quickly identify signs of dissection, particularly when access to advanced imaging such as CT is delayed or unavailable. With training, bedside ultrasound can help clinicians detect aortic root dilatation, pericardial effusion and other red flags that should prompt urgent escalation.
In 2021, Luke began working with the charity after the sudden loss of his mother-in-law from an undiagnosed aortic dissection. Since then, he has been instrumental in developing our education platform. His recent book, Point-of-Care Ultrasound in Critical Care, reflects his dedication to improving early recognition of serious conditions through practical, frontline tools.
The Role of Safe Transfer
Even with fast diagnosis, the journey to surgery is fraught with risk. Patients must be moved quickly, often across long distances. The ACCESS model offers hope. It sets a clear expectation that all transfers should be led by experienced critical care teams, with appropriate monitoring and blood pressure control. Patients should not be in the back of ambulances alone, without clinical escort or equipment.
Standardising this process across the UK is vital. It is one of the seven key principles in the NHS Acute Aortic Dissection Toolkit, developed in collaboration with TADCT. The ACCESS service shows that implementation is possible.
Driven by Lived Experience
Everything we do is shaped by the voices of patients and families. People like Valérie, who step forward to turn personal pain into public advocacy. People like Luke, whose personal loss drives his clinical leadership and commitment to improving diagnosis. When clinicians hear these stories directly, it changes the conversation.
It’s about people. About decisions made in pressure-filled moments. About the gaps we must close.