The Future of Aortic Care
Population-based studies, such as the Oxford Vascular Study (1) predict that cases of aortic dissection are set to rise over the next 10 years to more than 5,500 annually. If this trajectory comes to fruition, almost 3,500 people will lose their lives every year by 2050.
It’s vitally important to remember that aortic dissection is a treatable condition and has a better than 80% survival rate when it’s diagnosed and treated on time. Yet today, in 2022, 50% of people who are struck by this condition, die.
“We can’t carry on doing the same thing. It’s simply not good enough. We need to shape a safer future.”
Catherine Fowler BCAh – Trustee, The Aortic Dissection Charitable Trust

“We can’t carry on doing the same thing. It’s simply not good enough. We need to shape a safer future for those struck by this condition.”
Catherine Fowler BCAh – Trustee, The Aortic Dissection Charitable Trust
AD 2032 – The landscape for Aortic Dissection in 10 Years’ Time
At the 2022 SCTS Annual Meeting in Belfast, The Aortic Dissection Charitable Trust brought together leading experts to discuss their views on the future of aortic care. This summary of the session covers how genetics correlates to aortic disease, the surgical interventions of the future, and how a multidisciplinary team can care for patients and support the families affected by the condition.

In addition, a recent survey of patients on our aortic dissection research panel gave insight into what they would like to see over the next 10 years:
Diagnostics
A quick and simple blood test to reliably diagnose acute aortic dissection.
Treatment
That reduces the likelihood of requiring further intervention in the future.
Follow-up
That is regular and is always carried out by an aortic dissection specialist.
Genetic Screening
Proactive screening and identifying those at risk of an aortic dissection.
For us at the Aortic Dissection Charitable Trust, the future can’t come soon enough, and the charity will continue to play a proactive role in creating a safer future for people impacted by aortic dissection.
The Future of Surgical Interventions for Aortic Dissection
Professor Aung Oo – Consultant Cardiac Surgeon & Clinical Lead for Aortovascular surgery, Barts Heart Centre, Barts Health NHS Trust
To match the increasing incidence of aortic dissection, operations need to increase by 25% by 2030. There is little convincing evidence of a substantial increase in the number of operations over the past 5 years. Meeting the challenge of 2030 requires patients, surgeons, and the wider MDT to work together to improve this.
“The best way to build the future is to create it.”
Prof Aung Oo -Consultant Cardiac Surgeon & Clinical Lead for Aortovascular surgery

“The best way to build the future is to create it.”
Prof Aung Oo -Consultant Cardiac Surgeon & Clinical Lead for Aortovascular surgery
Limited aortic surgery of the past
Looking back 10 years ago, there was no dedicated aortic dissection rota across the UK. The strategy for dissection surgery, was limited with the main aim of surgery being to keep the patient alive with as short a stay in the hospital as possible, not to also prevent future complications. Only 4.7% of operations involved arch replacement surgery and only 20% an aortic root replacement. The frozen elephant trunk procedure was just becoming an option.
Post-repair surveillance was only being established and genetic counselling was not well integrated, therefore, post-operative complications and routine follow-ups were missed. Fortunately, today this has improved but still, not all patients benefit.
Aortic services has become more advanced
The service and expertise have improved in the past 10 years; the Liverpool and London Aortic Rotas have shown a halving in operative mortality. Aortic MDTs are now common and we have seen the introduction of the first aortic fellowship (first completed by Debbie Harrington).
Currently the strategy for aortic dissection surgery is more ambitious with an increasing range of graft options, such as the Thoraflex and AMD uncovered stent. To date, over 1,000 Thoraflex grafts have been implanted in the UK, with 35% used in acute aortic dissection cases. At the same time, better tools have been developed to help inspect the arch and understand the true and false lumen within the aortic wall tear which can often be less obvious on a CT scan.
More recently, the national coordination and organisation of aortic services promises to make a vast improvement for aortic dissection patients thanks to the NHS Acute Aortic Dissection Toolkit (launched in 2022), further development of the National Vascular Registry for aortic procedures, and the inclusion of patient and family opinions when selecting treatment options.
All of these initiatives will lead to a reduction in postoperative complications and the improvement of future treatment.
What the future of aortic dissection treatment will look like
The future care for aortic patients will genuinely be transformed when the NHS Acute Aortic Dissection Toolkit improves the traditional pathway for those suffering an aortic dissection.
However, everything from pre-hospital care to admission at the emergency department requires a nuanced review, including A&E triage processes, imaging, diagnosis, and transfer for surgery.
For a condition where every minute counts for patient survival, work needs to be done to reduce time to treatment. For instance, the diagnosis could be made pre-hospital, bypassing the emergency department with the patient being taken directly to the aortic centre in a similar way that is happening today for acute coronary syndrome and acute heart attack.
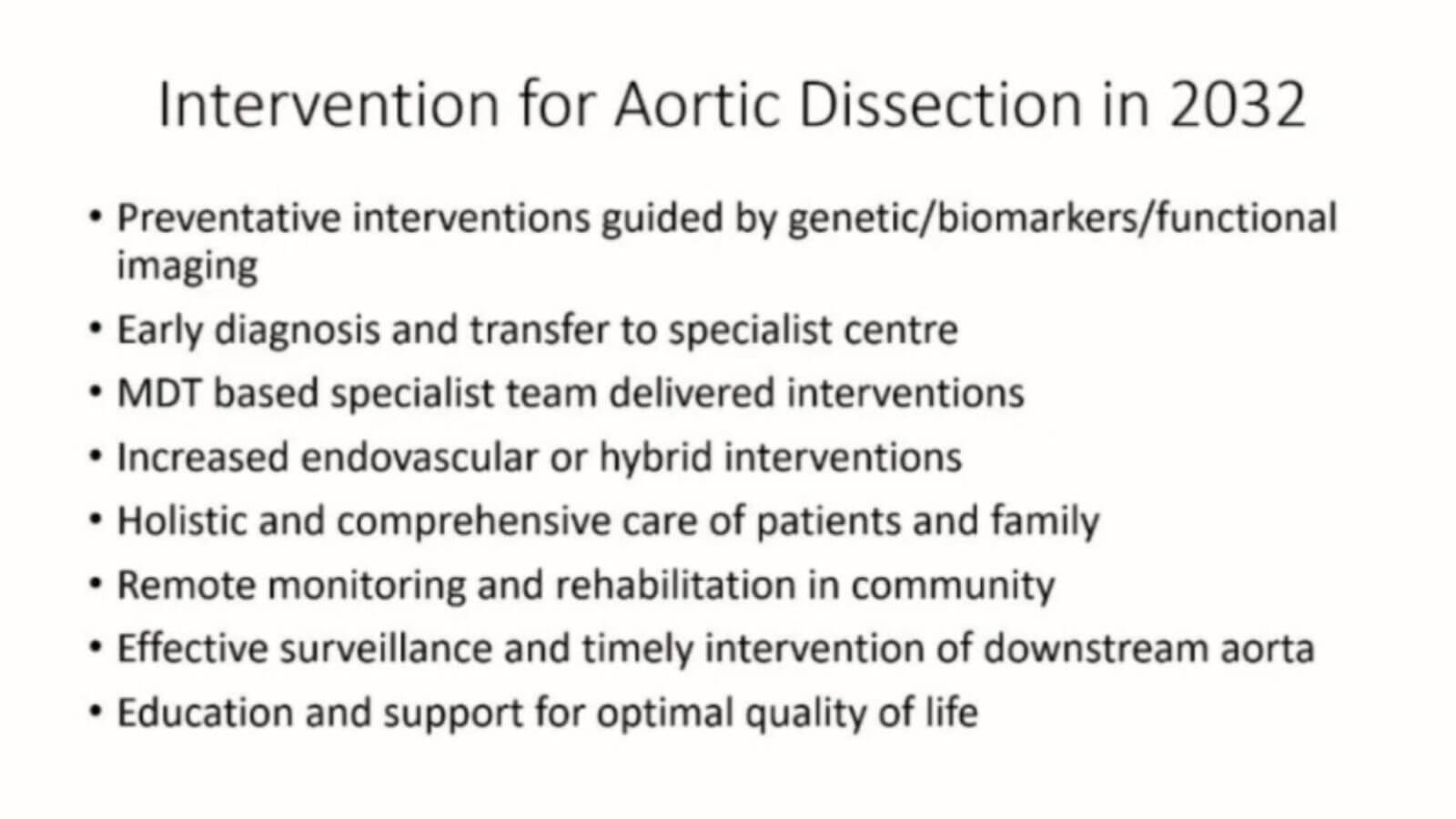
In addition the future will be improved by both increasing preventative aortic interventions guided by genetics, biomarkers and functional imaging (not just based on size only). And early diagnosis with an early transfer to a specialist centre where a multidisciplinary specialist team (MDT) can deliver the intervention with a range of endovascular and hybrid surgical options at their disposal.
Work also needs to focus on developing holistic and comprehensive patient care and support for their family. This includes, but is not limited to, improved patient education, remote monitoring options, personalised rehabilitation, effective surveillance, and timely intervention for potential secondary interventions or complications.
The focus is to support the patient and their family so they can enjoy an optimal quality of life after suffering from a dissection.
The Future of Genetic Testing for Aortic Dissection
Dianna M. Milewicz, M.D., Ph.D – Leading clinical geneticist at The University of Texas Health Science Center at Houston
Gene discovery and defining gene-based risk management
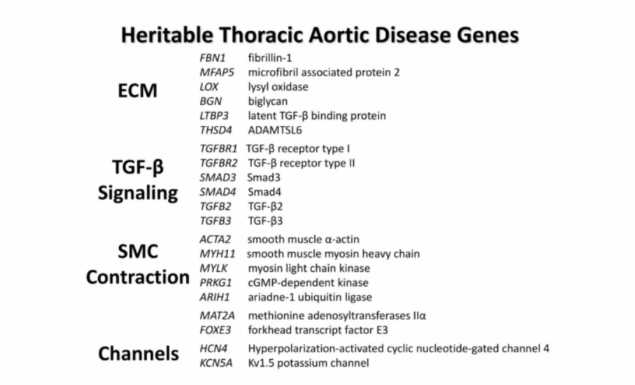
Genetic researchers have long known that an alteration in a single gene in the human genome results in a very high rate of thoracic aortic dissection; this gene being the FBN alterations. More recent studies have shown that up to 20% of families with thoracic aortic aneurysms or dissections pass down this single gene alteration through generations by autosomal dominant inheritance.
“The goal is to be able to identify individuals at risk in the general population early on.”
Dianna M. Milewicz, M.D., Ph.D – Leading clinical geneticist

“The goal is to be able to identify individuals at risk in the general population early on.”
Dianna M. Milewicz, M.D., Ph.D – Leading clinical geneticist
Imaging and surveillance of those at risk are recommended
This understanding of the genes helps identify individuals at risk for dissection. Once a patient is identified as having a family history of the disease, the recommendation is for genetic screening of all first-degree relatives.
The Texas team have been working for many years to identify the other genes that lead to aneurysms and dissections that are inherited within families. So far, 20-30% of those families with dissections have an identified gene.
Genetic heterogeneity is prevalent for this disorder, whereby different genetic mechanisms result in a higher risk of aortic aneurysm or dissection. This complexity makes standard genetic tools less sensitive in understanding the full genetic causes behind the condition.
Work continues in identifying the remaining 70-80% of the genetic causes. The ongoing hypothesis is that these genes have an individual low-risk, but when in combination with a second low-risk variant or an environmental (non-genetic) factor – such as hypertension, weightlifting, or long-term cocaine use – then the risk is increased and can lead to an aortic dissection.
The current research objective is to better understand what the genetic variants are, and the complete list of environmental factors that affect them. An example of this is the understanding of aortic toxins such as fluoroquinolone which is very much in an early stage.
Genome-wide association studies (GWAS), where the complete DNA samples of a large group of individuals are analysed for small gene variations, is one of the ways being used to identify genes that cause those low-risk predispositions. GWAS studies often end up identifying many of the same genes that cause familial disease. When these genes show up in patients where there is no family history, this is identified as a sporadic disease.
Artificial Intelligence
Machine learning is being developed as the next tool for genetic aortic disease risk prediction. Taking all that is currently known about the pathways involved in expressing the genes and external risk factors, it then uses this information to model the 80% of cases caused by sporadic disease. More work continues to improve the modelling, refining of control data, and utilisation of further pioneering clinical study data sources.

Biobank Studies
Using a larger set of historical data will help to better inform a risk prediction model on the analysis of aortic dissections in the sporadic population. The approach involves taking whole genome data from thousands of patients with confirmed dissections along with risk factor analysis of their medical records, such as the presence of a bicuspid aortic valve, family history, hypertension, prescribed medications, conditions such as diabetes and obstructive sleep apnoea. The model can then be applied to different cultural groups using local genomic data to produce a much more accurate global region population prediction to reduce premature death and disability due to acute aortic dissection.
Along with genome line sequencing and initiating lifestyle management, these advances will better help individuals at risk in the general population as well as identify those at risk early on, including young adults and even teenagers, to stop or minimise the non-genomic risk factors. Those at risk can then have surgical interventions to prevent a time-critical acute aortic dissection. This is the collective goal of global research teams.

Genetics Guiding Treatment
For the genes known to cause acute thoracic aortic disease, the worldwide collection of patient clinical data is being used to define the age of aortic event onset for each gene and recurring variants with the gene. Aortic events are defined as a patient presenting with a dissection or for a prophylactic repair. The results of this work in understanding the difference from gene to gene on the age of onset will help to inform treatment and keep patients one step ahead of the disease.
For example, with Marfan Syndrome, clinicians will monitor a change in the aorta and at five centimetres in diameter, can be fairly certain that the patient is at low risk for dissection, but with other genes, this is currently not possible. For some genes, repair of a completely normal aorta will be the preventative treatment of the future.
The future will see an easily accessible database available to healthcare professionals to support patient treatment. Treatment options will be based on the gene variant, enabling specialists to give tailored recommendations on medication and determine a variety of follow-up procedures such as how often they should image the patient’s aorta, whether arterial aneurysms need to be considered or further imaging for related conditions need to be carried out. For example, Moyamoya disease is one of the aortic gene variants that patients are at a predisposition to. Having an ever-evolving database like this will provide healthcare specialists with a pathway to treat patients more efficiently and effectively.
Join the UK & Ireland AD research panel
Would you like to support our research efforts to develop better treatments, more effective diagnostic tools and a deeper understanding of aortic genetics? Your insight and perspective as a person who has lived with AD or lost a loved one to the disease are invaluable.
The Future Aortic Care Team
Deborah Harrington – Consultant Cardiac & Aortic Surgeon at Liverpool Heart And Chest Hospital
Current diagnosis and treatment
In the UK & Ireland, for elective aortic surgery, most units are carrying out proximal aortic replacement and arch surgery. However, very few are carrying out descending thoracic aorta (DTA) and thoracoabdominal (TAAA) repairs.
For emergency and urgent surgery, all units carry out type A dissection repairs, but there are very few specialist rotas around the country, unlike the Liverpool Heart and Chest Hospital or the regional London aortic rotas.
Patients also face other issues in terms of diagnosis. The current pathways are ineffective and patients often go undiagnosed and are sent home. Radiology is not streamlined. There are problems transferring images. Other specialities often don’t consider aortic dissection and referral pathways are sporadic and complex around the country. Medical management, blood pressure control, imaging protocols, investigation of genetics, other related conditions, and long-term follow-ups are all sporadic and often not addressed well.
There is unwarranted variation in terms of the treatment of aortic disease around the country, too. There is variation in treatment rates per head of population and studies show that high-volume centres do have better outcomes.
“There is unwarranted variation in terms of the treatment of aortic disease around the country.”
Deborah Harrington – Consultant Cardiac & Aortic Surgeon

“There is unwarranted variation in terms of the treatment of aortic disease around the country.”
Deborah Harrington – Consultant Cardiac & Aortic Surgeon
A national strategy designed to improve services for patients

NHS England, along with patient support from The Aortic Dissection Charitable Trust, has produced the NHS Acute Aortic Dissection Toolkit which will significantly improve the pathway for AD patients and has the potential to save 500 lives annually and improve regional variation once implemented. This service change will run alongside the GIRFT (Getting It Right First Time) programme and is actively supported by patient advocates and SCTS as well as the UK Aortic Society.
Eliminating regional variation
The next step is for units to form regional acute dissection rotas, with a single point of contact to dramatically streamline aortic care across the UK and Ireland. In this situation, road and air ambulance transfers would be integrated, immediate diagnosis and medical management protocols would be embedded, and a backup plan would be in place to cover on-call units already dealing with acute dissection cases.
These regions need to have full MDTs in place that is coordinated with regular open dialogue between centres to support service improvement, aortic education, and patient research. There needs to be coordination and funding for that coordination.
The Liverpool Heart and Chest Hospital approach
Liverpool has had a local aortic rota with a faculty of specialist aortic surgeons since 2007. The aortic surgeons perform all the elective aortic dissection repairs with the service developing further with subspecialist teams to support ongoing and improved patient care.
Liverpool has multiple MDTs with a growing and consistent training programme as well as a programme to develop aortic fellows. The aortic centre runs regular dual consultant operations to allow everyone to train using the latest aortic interventions to ultimately improve patient outcomes.
The aortic programme at Liverpool has been expanding over the past 10 years. With a vision to embed best practice, patient-centred care that is personalised for each patient with seamless pathways supported at every step.
The team at Liverpool includes surgeons, cardiac surgeons, vascular surgeons, physicians, cardiologists, aortovascular physicians, imaging specialists, geneticists, and radiologists. Team members also include allied health professionals, nursing advanced nurse practitioners, specialist surgical care practitioners, MEP technicians, and MDT coordinators. More recently, the addition of psychologist services to support patients and families with PTSD following acute dissection.
So, what will the dissection pathway of the future look like?
The Aortic Dissection Charitable Trust are working to improve diagnosis through education and raising awareness so that every emergency department will consider aortic dissection. The aim is that patients will undergo a CT scan of the whole aorta, which will be immediately reported and transferred to the appropriate aortic centre. The aortic team on call will be contacted via a single point of contact. The patient will immediately be blue light transferred to the aortic centre where they will be admitted straight to theatre.
Post-diagnosis there will be in place long-term and streamlined follow-up covering genetic investigation, family screening, and psychological support for patients and their families with input and oversight from aortovascular specialists. These aortopathy clinics will combine vascular, aortic and genetic specialists to support the patients and their families diagnosed with an aortopathy.
Centres will have specific genetic clinics to screen patients and their families for aortic genes associated with aortopathy. Provisions will be made to have a dedicated aortic nurse practitioner clinic assist with aneurysms and other high AD-risk patients.
The future aortic MDT will accommodate distal and proximal expertise as well as structural heart specialists to support complex valve repair and high-risk endocarditis patients. A team that will be able to respond to all urgent cases.
What about education?
It’s vital that surgeons are given the tools through masterclasses and training courses to be able to operate on the most complex of patients in the hardest of situations. It’s important that A&E departments and other medical specialities, including paramedics, are aware of aortic dissection. Medical students need to know about aortic disease and dissection because if they haven’t encountered it during their studies, they probably won’t consider it later in their careers.
Patients and families need to be fully informed from the start, so they can look out for symptoms, determine if they are at risk, and what treatment and follow-up procedures they can come to expect.
Ideally, there should be a national aortic fellowship in place, which is SAC (Specialty Advisory Committee) approved, like the current transplant and congenital fellowships. This should come with training programmes developed specifically for proximal, distal and interventional phases, which run concurrently with existing education.
Type-A aortic dissection. Story was opposite of textbook. Normal labs, EKG, CXR, vitals, exam. Pain improved with massage. Couldn’t shake my gut feeling. CTA was positive.
— Liz Calhoun, MD, FAAEM (@ecalhoun21) October 22, 2022
Flown out. Got a text he lived neuro-intact despite prolonged time on bypass.
There are many areas of the aortic pathway where further development needs to happen. Epidemiological studies, biomechanics, operative techniques, follow-up, and genetics are all aspects covered here. Ultimately, a national network of MDTs must be assembled, so that patients with aortic disease can receive the treatment and care they deserve.
References
1. Howard P, Banerjee A, Fairhead J et al. Population-Based Study of Incidence and Outcome of Acute Aortic Dissection and Premorbid Risk Factor Control 10-Year Results From the Oxford Vascular Study. Circulation. 2013;127:2031-2037


Privacy Policy | Accessibility
The Aortic Dissection Charitable Trust
Registered charity in England & Wales No. 1191420
Registered charity in Scotland No. SC051517
PO Box 812, Hope Valley, Chesterfield S40 9QY
The information and materials on this site are for general information purposes only. This site is not designed to provide individual medical advice, diagnosis or treatment. If you have any concerns, please speak to your GP. If you believe you have a medical emergency, call 999 immediately.